Do Physicians Use Marijuana?
Carol Peckham
DisclosuresFebruary 05, 2015
Marijuana Usage in Physicians
The
Medscape Lifestyle Report 2015 included questions on physicians' use of marijuana and their opinions on legalization. Other surveys have been conducted on physicians' attitudes toward medical marijuana, but very few have asked about doctors' own history of usage. A 2013 Gallup poll
[1] reported that 38% of Americans have tried marijuana, a percentage that has increased by only 5% since 1985. Only 7% say they are currently using it. In this year's Medscape survey, physicians report a lower rate of history of marijuana use, with just under a quarter reporting ever having tried it. Three percent say they've used marijuana in the past year, also a lower percentage than that found in the Gallup poll for the general population.
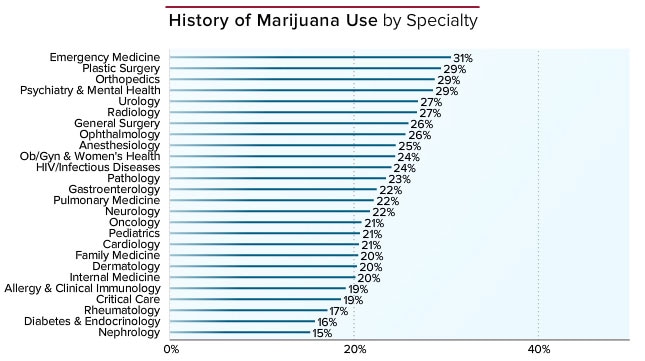
There is no difference in marijuana usage between burned-out and non–burned-out physicians. There is also very little difference in usage between male (25%) and female (21%) physicians (Figure 1).
Figure 1. History of marijuana use by gender.
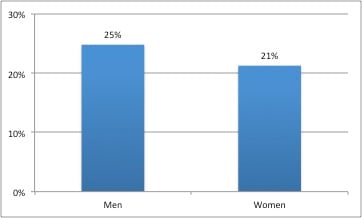
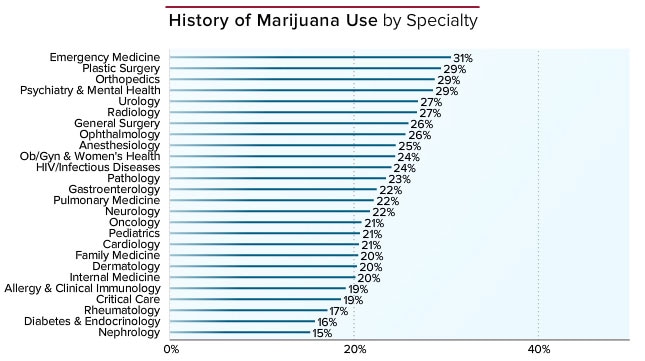
Marijuana history varies somewhat by specialty, however (Figure 2). In this survey, emergency medicine physicians report the highest history of marijuana use (31%), followed by plastic surgeons, orthopedists, and psychiatrists at 29%. The least likely to report ever using marijuana are nephrologists (15%), endocrinologists (16%), and rheumatologists (17%).
Figure 2. Marijuana use by specialty.
 Physician Use of Marijuana and Alcohol
Physician Use of Marijuana and Alcohol
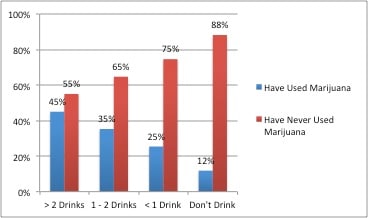
A study of French medical students found an association between high-risk alcohol and high-risk cannabis consumption but no correlation with anxiety or depression.[2] The Medscape 2015 report echoed these results, finding a correlation between higher levels of alcohol consumption and a greater tendency to have used marijuana, although there was no association between burnout and usage of either of these substances. Of those who have more than two alcoholic beverages per day, 45% claim to have ever used marijuana. The less physicians drink, the less likely they are to have used marijuana; only 12% of those who don't drink at all claim to have ever used marijuana (Figure 3). It is worth emphasizing that Medscape physician responders report very light to moderate drinking habits; just under a third of all physician responders said they didn't drink at all, and about half claimed having less than one drink per day.
Figure 3. Marijuana and daily alcohol use.
Physician Age and Marijuana Use
According to the Gallup poll, when filtered by age, 49% of Americans ages 30-49 years and 44% of those 50-64 years have used marijuana at some point; the youngest and oldest groups had the lowest percentages (36% and 17%, respectively).
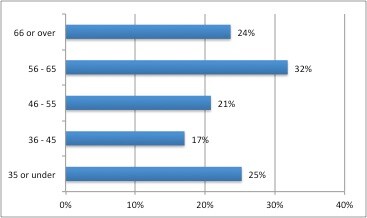
[1] Usage by age differs slightly among physicians who responded to the Medscape survey (Figure 4). The highest usage rate (32%) is among the baby boomers, ages 56-65. It drops considerably in the next two younger age groups, with 21% of those 46-55 and only 17% of those 36-45 reporting use. That number rises again among the youngest physicians (under 35) to 25%.
Figure 4. Physician marijuana history by age group.
This pattern—peak history of usage in midlife, then a decline in younger physicians, followed by a rise in the youngest doctors—reflects a general trend reported in a national survey
[3] that has tracked substance abuse over several decades in the general population. In the latest report on this survey, those in their 50s tended to be a "very drug-experienced segment of the population, as might be expected due to the fact that they graduated from high school near the peak of the drug epidemic." The authors then observed a decline in drug-taking in the next younger age groups, who had a greater perceived sense of risk during the years when they were growing up. The survey is now reporting an increasing trend of drug-taking in college students, which they attribute to "a generational forgetting of those risks ... through a process of generational replacement of older, more drug-savvy cohorts with newer, more naive ones." According to recent government data, marijuana use is declining in high-school adolescents.
[3,4]
Legalizing Medical Marijuana
Alcohol was once illegal because of its devastating effects from addiction and the deleterious impact of heavy use on the body and the brain. Although these harmful effects remain, our culture is at ease now with alcohol's legality and recreational use. This is one argument for the legalization of marijuana, which so far has not been demonstrated to exhibit harmful effects as severe as those of alcohol, even with long-term use.
Increasing evidence shows that, compared with many other pharmaceutical interventions, marijuana used in medical treatments is relatively safe. In the United States, 22,134 deaths related to pharmaceuticals and 9429 additional deaths from the use of unspecified drugs were recorded in 2010.
[5] According to recent data from the Centers for Disease Control and Prevention (CDC), no deaths caused by medical marijuana overdose have been confirmed in the United States.
[6]In fact, a report in
JAMAconcluded that there are 25% fewer opioid overdose deaths each year in states where access to medical marijuana is legal, compared with states where it is not. Death rates decreased dramatically in the years immediately after legalization.
[7]
However, it is naive to justify legalizing marijuana's recreational use simply on the basis of its relative safety compared with alcohol and other drugs. Cannabis, taken recreationally or medically, is still a drug. And any drug with beneficial effects also has harmful ones. Furthermore, no one is certain what the actual benefits—and, conversely, full harm—from marijuana may be.
The American Medical Association acknowledged some therapeutic benefits of cannabis in a policy statement
[8] but added, "The patchwork of state-based systems that have been established for 'medical marijuana' is woefully inadequate in establishing even rudimentary safeguards that normally would be applied to the appropriate clinical use of psychoactive substances. The future of cannabinoid-based medicine lies in the rapidly evolving field of botanical drug substance development, as well as the design of molecules that target various aspects of the endocannabinoid system. To the extent that rescheduling marijuana out of Schedule I will benefit this effort, such a move can be supported."
Positions on Legalization by Specialty
A 2014 Gallup poll reported that over half (51%) of Americans support legalization.
[9] Among physicians who responded to the current Medscape survey, 59% of those who have ever used marijuana support total legalization, and 20% support it only for medicinal purposes. Even among physicians who have
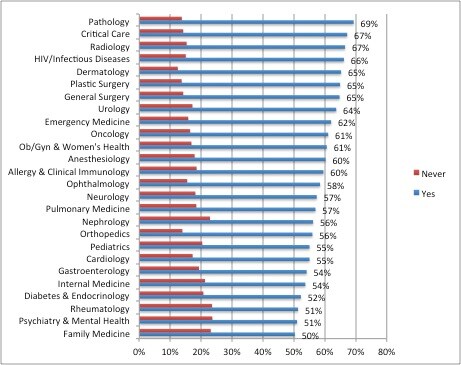
never used marijuana, 51% support some form of legalization (23% total and 28% medicinal). Positions on marijuana legalization vary somewhat by specialty (Figure 5).
Pathologists, at 69%, and intensivists and radiologists, at 67%, were the most favorable toward some degree of legalization. Family physicians hold the least favorable view on marijuana legalization, with half of them supporting legalization of some form and nearly a quarter (23%) saying it should never be legalized. (The remaining FPs remained uncertain.) The American Academy of Family Physicians does not endorse legalization but urges its members to be knowledgeable about their state laws and consult with state medical boards on guidance for the use of medical marijuana.
[10]
Psychiatrists who responded to the Medscape survey were the second least likely specialty to advocate legalization, with only 51% favoring legalization and 24% completely opposed to it. (Of interest, 29% of psychiatrists reported a history of usage, which was fourth from the top among all physicians.) The American Psychiatric Association has also come out against legalization of marijuana, at least until it has been well investigated, particularly given its potential harm on adolescent users.
[11]
Some research offers promise on treating specific conditions (eg, multiple sclerosis, inflammatory bowel disease, and fibromyalgia), but there is less acceptance of legalization than might be expected among physicians in specialties that treat these conditions. These specific conditions, and the evidence for use of marijuana in treating them, will be discussed in more detail later.
There is some institutional support for the use of cannabis in treating symptoms of multiple sclerosis, so one might expect that more than 57% of neurologists responding to our survey would favor some form of legalization.
Marijuana has anti-inflammatory properties, and some research suggests that it is helpful in relieving inflammatory bowel disease symptoms and irritable bowel syndrome. However, in our survey, only 54% of gastroenterologists support legalization, perhaps because of the lack of well-controlled randomized studies.
There is limited evidence that marijuana can relieve symptoms in patients with fibromyalgia, but no studies to date have found it to be of benefit in treating arthritic pain. This may explain why rheumatologists, at 51%, were among the three specialties least likely to support legalization.
Figure 5. Marijuana legalization support by specialty.
Physician Usage and Views on Legalization by Region
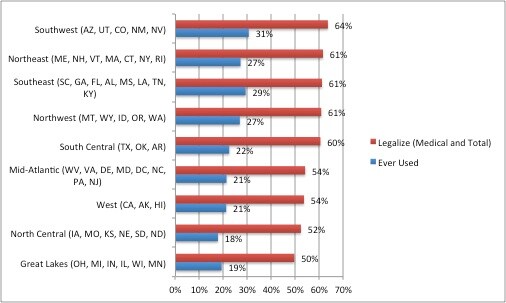
Analyzing physician opinions by region demonstrates that marijuana usage and support for legalization go hand in hand (Figure 6). But do the highest percentages of physician support for either medical or total legalization always occur in states where marijuana is now legal in some form?
[12]
A 2014 Gallup poll reported that among all Americans, the greatest level of support of legalization, at 57%, is in the East and the West.
[9] Physicians in the Southwest, which has four states where medical marijuana is legal, report both the highest rate of history of usage (31%) and the most positive view toward legalization (64%). The Northeast, where all of the states have some form of legalization, holds the second spot for physician support of legalization (61%). However, in the Southeast, marijuana is not legal in any of its states, and yet an identical 61% of its physicians also support legalization. Notably, usage history (29%) in the Southeast is actually higher than in the Northeast (27%). Furthermore, physicians who live in the Great Lakes area, where half of the states have some form of legalization, are at the bottom of the list in support for legalization (50%) and second to the bottom in usage history (19%). The North Central region, which has no states with legalization laws, is second from the bottom for support of legalization, with 52% of physicians favoring it and only 18% having ever used marijuana.
Figure 6. Physician history of use and legalization support by region.
Medical Uses of Marijuana
In 2013, the
New England Journal of Medicine presented its readers with a case study of Marilyn, a 68-year-old woman with metastatic breast cancer, and asked whether they would prescribe marijuana to help alleviate her symptoms; 76% responded positively.
[13] A Medscape
poll of clinicians regarding medical use of marijuana, conducted in 2014, found similar support for a therapeutic role for cannabis. About 70% of physicians believed that marijuana had real medical benefits, although only 1% had ever used it for medicinal purposes themselves.
Two cannabis-derived pharmaceuticals are available in the United States and Canada: dronabinol (schedule III) and nabilone (schedule II). A third, nabiximols, is available in Canada but is not approved by the US Food and Drug Administration. Both the Institute of Medicine and the American Medical Association have supported the therapeutic benefits of cannabinoids for pain relief, control of nausea and vomiting, appetite stimulation (particularly among cancer patients), and for reducing pain and spasticity in patients with multiple sclerosis.
[8,14] The American Academy of Neurology has also just released guidelines for using cannabis in treating multiple sclerosis.
[15]
Nevertheless, healthcare workers face complicated and as yet unresolved issues related to cannabis as therapy. The legalization of marijuana for recreational or medical use in a number of states now provides the opportunity to study its effects—beneficial or harmful—in more substantive ways than previously, which ultimately will help the clinician to make decisions about cannabis use in practice.
Treatment of Non-cancer Chronic Pain
Cannabinoids appear to have some benefit in relieving neuropathic pain.
[16-19] Preliminary recommendations have been issued from the College of Family Physicians in Canada to help guide clinicians in prescribing cannabis for this purpose.
[20] To date, however, most research does not indicate a similarly favorable risk-benefit ratio for marijuana's use in relieving arthritic pain.
[21-23] Some evidence suggests that cannabis may reduce the need for opioids in patients with chronic pain, although most of these studies are based on patient self-reports.
[24] One small study in 2011
[25,26] suggested that in patients taking long-acting opioid analgesics for various chronic pain conditions, a potential combination treatment with vaporized cannabis could reduce pain and might also cut opioid dosing.
Multiple Sclerosis
Cannabis is being used in the management of pain and spasticity from multiple sclerosis, although evidence of its value is still limited.
[27-30] Despite the current state of evidence,
[31] the American Academy of Neurology released guidelines in 2014 on its use in treating patients with multiple sclerosis.
[15]
Cancer
Dronabinol and nabilone are indicated for the treatment of nausea and vomiting associated with cancer chemotherapy and anorexia associated with weight loss.
[32] Although evidence to date of marijuana's effectiveness in relieving symptoms of cancer (pain, nausea and vomiting, loss of appetite, and weight loss) have been inconclusive, recent studies are promising.
[33,34] Some interesting research suggests that cannabinoids may have an antiproliferative effect on tumors of different origin, which bears clinical investigation.
[35,36]
Inflammatory Bowel Disease and Other Gastrointestinal Conditions
Because of its anti-inflammatory properties and effects on motility, cannabis preparations are considered promising tools for the management of inflammatory bowel disease and other gut disturbances.
[37-40]
Neuropsychiatric Effects
The neuropsychiatric effects of marijuana are of particular concern and still not yet fully known. Of interest, in Colorado, physicians who legally use medical marijuana to treat their own conditions are considered unsafe to practice until they no longer need such treatment. (The use of other substances, such as alcohol or sedating medications, does not preclude Colorado doctors from practicing.)
[41]
Neurocognitive performance. An 8-year study
[42] and a meta-analysis
[43] found that marijuana had few long-term effects on learning and memory. The meta-analysis reported that "any negative residual effects on neurocognitive performance attributable to either cannabis residue or withdrawal symptoms are limited to the first 25 days of abstinence. Furthermore, there was no evidence for enduring negative effects of cannabis use."
Recently, however, a large study found neuropsychological decline in adults who had been heavy users of marijuana in their adolescence.[44] In addition, stopping the drug did not prevent further decline. Further studies are needed. To offer some perspective, research to date finds the effects of heavy alcohol use on young people's brains to be far more detrimental than those of marijuana. In fact, some research suggests that marijuana might be somewhat neuroprotective in young users of alcohol.[45,46] It should be strongly stressed, however, that young brains are vulnerable to the negative, even long-term, effects of all substances that affect the brain, including marijuana.
Addiction. Contrary to the views of many of its proponents, research suggests that a quarter to a half of those who use marijuana daily are addicted to the drug.
[47]
Mood disorders and psychosis. The effects of marijuana on depression and anxiety are unclear. A longitudinal study found no association with mood disorders, although it did find higher incidences of bipolar disorder.
[48] Other evidence supports an association between marijuana use and a higher risk for future development of psychotic symptoms, but the link is contentious.
[49-52] A 2014 study on post-traumatic stress disorder suggested that concomitant use of medical marijuana nullified the benefits of existing treatment in these patients.
[53]
On a more favorable note, a 2015 regression analysis reported a lower suicide rate in young men in states where medical marijuana was legal, compared with the rate in states where it wasn't. The authors believe that it is the first study to examine the relationship between marijuana and suicides. The study could not establish a causal relationship, of course. Another factor that could play a part in the decrease in suicides was the reduction in alcohol use in those states where marijuana was legal.
[54]
Cardiovascular Effects
Research is now pointing to adverse cardiovascular effects from cannabis use, including myocardial infarction, sudden cardiac death, cardiomyopathy, stroke, transient ischemic attack, atrial fibrillation, and cannabis arteritis.
[55-57] For example, in a French study, 1.8% of adverse effects reported from cannabis use were cardiovascular complications, which were associated with a death rate of 25.6%.
[58]
Pulmonary Effects
The effects of smoking marijuana on lung function are unclear, partly because most users also smoke tobacco.
[59] Lung cancer studies to date largely do not support an association with marijuana use, possibly because of the smaller amounts of marijuana regularly smoked compared with tobacco.
[60,61] There may be a risk, however, in heavy users.
[62, 63]
Accidental Overdose in Children and Young People
After marijuana was legalized in Washington State, marijuana poisonings spiked in adolescents.
[64] In January 2015, a leading anti-marijuana group reported an increase in the number of children treated for accidental marijuana consumption in Colorado as well, and a surge in the numbers of adolescents treated for cannabis abuse.
[65] "Trying to draw any conclusions with less than 1 year of data is irresponsible," pro-cannabis Marijuana Policy Project spokesman Mason Tvert said. In addition, if alcohol use is declining in these states, it would be important to determine whether there is also a decline in treating alcohol use or other forms of drug abuse that might offset the increase in cannabis abuse treatment. In a
policy statementissued in January 2015 reaffirming opposition to legalization of marijuana, the American Academy of Pediatrics recommended that where it is legal, regulations should be enacted to insure that all product is distributed in childproof packaging to prevent accidental ingestion.
[66]







 EMail
EMail Print
Print Twitter
Twitter Facebook
Facebook Reddit
Reddit Google+
Google+